Session 4: Walking with the Pelvic Floor
- csnijdersvw

- Oct 5, 2024
- 4 min read
Updated: Dec 5, 2025

The territory of session 4 of the Series covers the core structures of the lower body, paying particular attention to the pelvic floor and its support and connections through the legs. The pelvic floor may be an area that you hardly know exists, or perhaps you are all too aware of it.
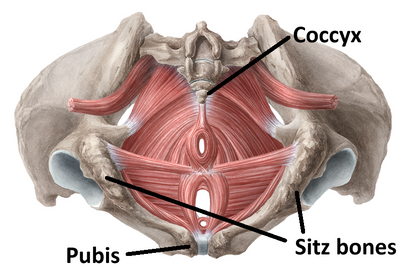
The pelvic floor is a group of muscles and connective tissues that span the space within the pelvis between the pubic bone, sacrum and coccyx, and sitz bones. These soft tissues form the bottom of the abdominal cavity, so they provide important support to the organs above and the tubes running through. They also play important roles in urination, defecation, sex, and reproduction.
Pelvis viewed from above (left) and below (right):
Pelvic Floor Dysfunction (PFD) is a category of symptoms resulting from any part of the pelvic floor functioning abnormally. This can include muscles being too tight, too loose, or not coordinating together. Anyone who has a pelvic floor (which is every person) can have PFD. Factors that can make PFD more likely include:
· Increased age
· Having had surgery in the abdomen or pelvic region
· Chronic increased pressure within the abdominal cavity
· Chronic stress
· Having given birth
· Having a sedentary lifestyle
Symptoms of pelvic floor dysfunction can be widely varied. These may include:
· Problems with urination, such as incontinence or urgency
· Problems with defecation, such as incontinence or constipation
· Pain anywhere in the pelvic region
· Pain or difficulty with having sex
· Any amount of pelvic organ prolapse
· Herniations or bulging of any of the pelvic structures, such as bladder, urethra, uterus, rectum, or intestines
· Pain in the low back, buttocks, abdomen, or legs
The cause of pelvic floor dysfunction is often not straightforward. The pelvic floor exists in relationship to the rest of the structures connecting with the pelvis, of which there are many. Habitual postures and movement patterns commonly develop imbalance in the pelvis slowly over time. Big events like an injury or challenging birth experience can also quickly change the environment in which the pelvic floor resides.
One of the issues we can deal with, whether or not we have PFD, is weakness of the pelvic floor muscles. They should respond, but they don’t. One method of teaching them to respond appropriately is to learn to do Kegels. Kegels are an exercise that you can learn with a physical therapist or other professional to specifically be able to engage and relax your pelvic floor muscles. However, this addresses just one part of the picture.
It is important for longer-term wellness to balance the structures around the pelvis. When pelvic floor muscles are weak, sometimes they need to learn how to engage and tighten up again. Conversely, they may seem weak because they are already so tight that they can’t respond any further. If you close your hand into a fist, at a certain point you can no longer squeeze your hand any more tightly. This is the situation that many pelvic floors are in.

The pelvic floor muscles normally exert a pull on the pubic bone and sacrum in a similar fashion as a trampoline pulling on its supports. In some situations, the PF muscles pull so much that they move the sacrum in, changing the shape of the pelvis and affecting their ability to do their jobs. How do we balance all this tension inside the pelvic bowl?
The pelvic floor muscles attach to the inside of the pelvic bowl. The glute muscles attach to the outside. Together, the glutes and pelvic floor balance each other in relation to the bones they hold.

When the glutes and other muscles around the pelvis are balancing the tension exerted by the pelvic floor, adequate space is held for everything to do its job properly. Here are some ways that we can diminish the availability of the glutes and posterior pelvis structures to do their jobs:
· Sitting a lot, especially when we put our weight on the sacrum rather than sitz bones
· Spending more time being sedentary, such as sitting or standing rather than walking
· Wearing shoes with elevated heels
· Having pelvic alignment that inhibits the glutes from working while walking
The above situations often lead to tension in the back of the legs, weakness in the glutes, and a posteriorly tilted pelvis, which means the pelvic bowl is tipped behind you and your tailbone is tucked under you. They can’t do their jobs because they don’t have the space to operate.
The alignment of the pelvis has a big influence on how the glutes, pelvic floor, and other lower body muscles will function. When we wear heeled shoes, we are standing on a downward slope. It is normal to sometimes stand on downward sloping terrain but not for every moment you are up and about. Even if the heels of your shoes are not that big, they will create an effect on the rest of your body alignment.

When the pelvis is posteriorly tilted, the hips have less room to extend. This means you can’t pull your legs behind you as you walk, so you don’t work your glute muscles and your pelvic floor doesn’t have an equal force to balance it.

These are just a few ways that your pelvic floor is connected to the rest of your body and the ways you are moving. The main point is that your pelvic floor doesn’t exist in a vacuum. It’s an important part of the beautiful, complex organism that is you. Including this region in your awareness of yourself, moving your whole body dynamically each day, seeking balance in the structures that surround your pelvis—these are the ways to nourish your pelvic floor.